Introduction
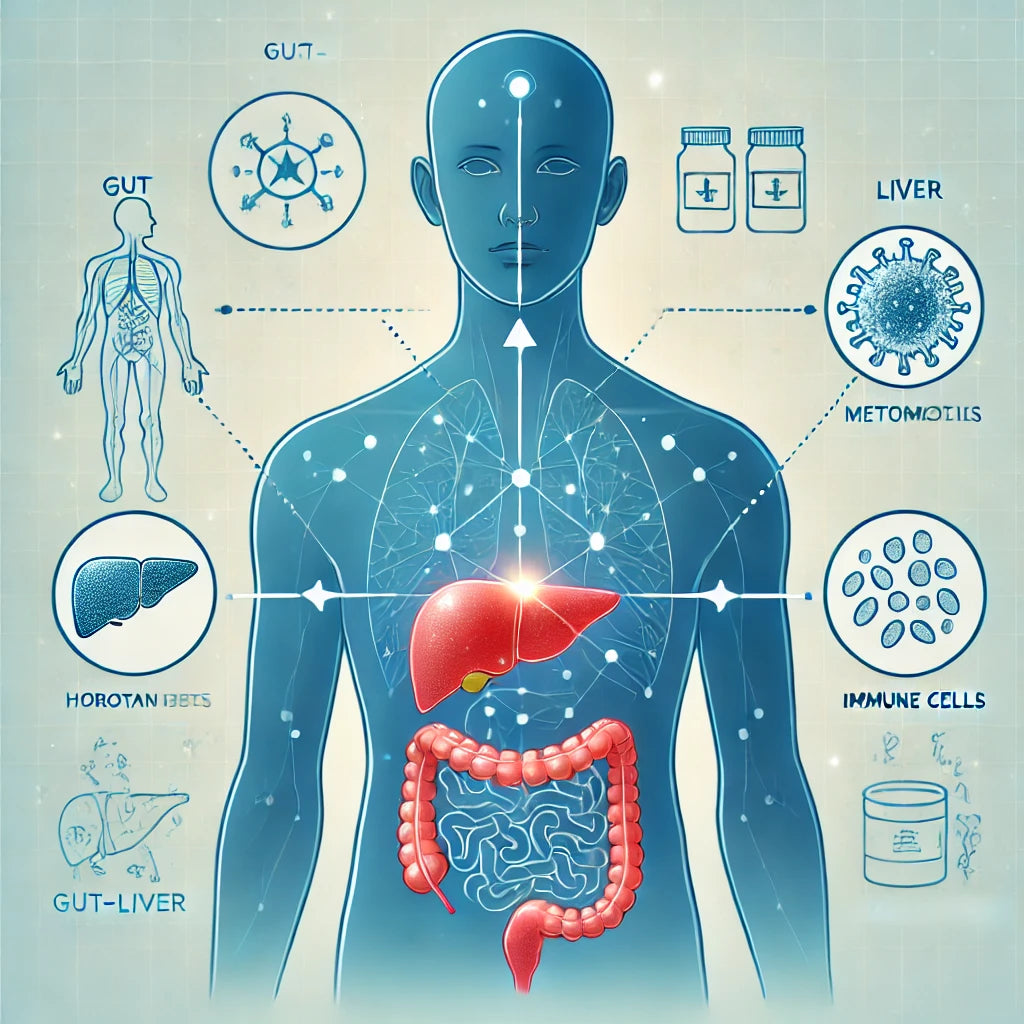
The intricate relationship between the gut and the liver, known as the gut-liver axis, plays a vital role in maintaining overall health. This connection, facilitated by complex biochemical signaling pathways, influences various physiological processes, including digestion, metabolism, and immune response. In this blog post, we delve into the concept of the gut-liver axis, its functions, and its implications for health and disease.
The Gut-Liver Axis: An Overview
The gut-liver axis refers to the bidirectional communication network between the gastrointestinal tract and the liver. This axis is mediated by the portal vein, which transports nutrients, metabolites, and microbial products from the gut to the liver, and by various signaling molecules that travel through the bloodstream.
- The Portal Vein: A major blood vessel that carries nutrient-rich blood from the intestines to the liver.
- Microbial Metabolites: Compounds produced by gut microbiota, including short-chain fatty acids (SCFAs), bile acids, and lipopolysaccharides (LPS), which influence liver function.
Functions of the Gut-Liver Axis
The gut-liver axis is crucial for numerous bodily functions, including:
-
Nutrient Metabolism
- Carbohydrate and Lipid Metabolism: The liver processes nutrients absorbed from the gut, playing a key role in glucose and lipid metabolism.
- Vitamin and Mineral Storage: The liver stores essential vitamins and minerals, such as vitamin A, D, E, K, and iron.
-
Immune Regulation
- Immune Surveillance: The liver contains a large population of immune cells that monitor and respond to antigens from the gut.
- Inflammatory Response: Gut-derived microbial products can trigger inflammatory responses in the liver, influencing overall immune function.
-
Detoxification
- Toxin Neutralization: The liver detoxifies harmful substances absorbed from the gut, protecting the body from potential damage.
- Drug Metabolism: The liver metabolizes medications, influencing their efficacy and toxicity.
The Gut Microbiome and Liver Health
The gut microbiome, comprising trillions of microorganisms, significantly impacts liver health through the gut-liver axis. A balanced microbiome supports liver function, while dysbiosis—an imbalance in the microbial community—can lead to various liver diseases.
Role of the Gut Microbiome
- Microbial Diversity: A diverse microbiome is associated with better health outcomes, including improved liver function.
- Metabolite Production: Beneficial microbes produce SCFAs and other metabolites that promote liver health by reducing inflammation and supporting metabolic processes.
Dysbiosis and Liver Diseases
- Non-Alcoholic Fatty Liver Disease (NAFLD): Dysbiosis can contribute to NAFLD by promoting inflammation, insulin resistance, and fat accumulation in the liver.
- Alcoholic Liver Disease (ALD): Excessive alcohol consumption disrupts the gut microbiome, leading to increased gut permeability, endotoxemia, and liver damage.
- Liver Cirrhosis: Chronic liver diseases can result in cirrhosis, characterized by severe liver scarring. Dysbiosis exacerbates liver inflammation and fibrosis.
Mechanisms Linking the Gut and Liver
Several mechanisms underlie the gut-liver axis, including:
-
Microbial Translocation
- Increased Gut Permeability: Dysbiosis can increase intestinal permeability, allowing microbial products like LPS to enter the bloodstream and reach the liver.
- Immune Activation: These microbial products can activate immune cells in the liver, triggering inflammation and contributing to liver disease.
-
Bile Acid Metabolism
- Bile Acid Synthesis: The liver produces bile acids, which aid in digestion and regulate gut microbiota composition.
- Microbial Modification: Gut bacteria modify bile acids, influencing their signaling roles and impacting liver metabolism and inflammation.
-
Metabolic Endotoxemia
- LPS and Inflammation: Lipopolysaccharides (LPS) from gut bacteria can induce systemic inflammation, affecting liver function and promoting metabolic disorders.
Implications for Health and Disease
Understanding the gut-liver axis opens new avenues for diagnosing, preventing, and treating various diseases. Key implications include:
-
Diagnostic Biomarkers
- Microbial Signatures: Specific microbial patterns can serve as biomarkers for liver diseases, aiding in early diagnosis and personalized treatment strategies.
- Metabolite Profiles: Analyzing microbial metabolites can provide insights into liver health and disease states.
-
Therapeutic Interventions
- Probiotics and Prebiotics: Supplementing with beneficial bacteria (probiotics) or compounds that promote their growth (prebiotics) can restore microbial balance and improve liver health.
- Fecal Microbiota Transplantation (FMT): Transplanting fecal bacteria from healthy donors to patients can reset the gut microbiome, offering potential benefits for liver disease treatment.
-
Diet and Lifestyle Modifications
- Dietary Fiber: High-fiber diets support a healthy microbiome and reduce the risk of liver diseases by promoting the production of SCFAs.
- Reduced Alcohol Intake: Limiting alcohol consumption can prevent alcohol-induced dysbiosis and subsequent liver damage.
Future Directions in Gut-Liver Axis Research
Research into the gut-liver axis is rapidly evolving, with promising future directions including:
- Personalized Medicine: Tailoring treatments based on individual microbiome profiles to optimize liver health.
- Microbiome-Based Therapies: Developing targeted therapies that modulate the gut microbiome to prevent and treat liver diseases.
- Advanced Diagnostics: Utilizing next-generation sequencing and metabolomics to identify early biomarkers of liver disease and monitor treatment responses.
Conclusion
The gut-liver axis is a critical component of human health, influencing various physiological processes and disease states. By understanding the complex interactions between the gut microbiome and the liver, we can develop innovative strategies for preventing, diagnosing, and treating liver diseases. Maintaining a healthy gut microbiome through diet, lifestyle, and potentially targeted therapies holds promise for enhancing liver health and overall well-being.
As research continues to uncover the nuances of the gut-liver axis, we can look forward to new insights and therapeutic approaches that harness the power of the microbiome in promoting liver health and preventing disease. Embracing this holistic perspective on health can lead to more effective and personalized medical care, ultimately improving outcomes for patients with liver and related diseases.



